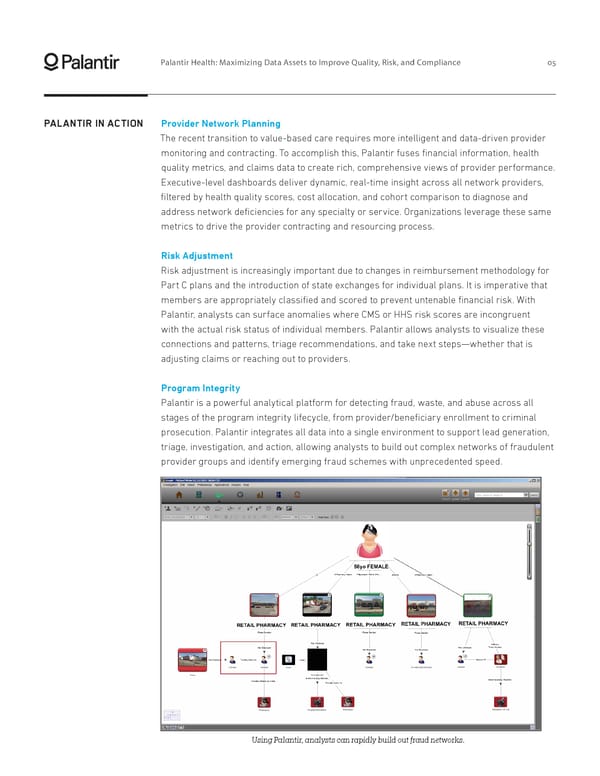
Palantir Health: Maximizing Data Assets to Improve Quality, Risk, and Compliance 05 PALANTIR IN ACTION Provider Network Planning The recent transition to value-based care requires more intelligent and data-driven provider monitoring and contracting. To accomplish this, Palantir fuses financial information, health quality metrics, and claims data to create rich, comprehensive views of provider performance. Executive-level dashboards deliver dynamic, real-time insight across all network providers, filtered by health quality scores, cost allocation, and cohort comparison to diagnose and address network deficiencies for any specialty or service. Organizations leverage these same metrics to drive the provider contracting and resourcing process. Risk Adjustment Risk adjustment is increasingly important due to changes in reimbursement methodology for Part C plans and the introduction of state exchanges for individual plans. It is imperative that members are appropriately classified and scored to prevent untenable financial risk. With Palantir, analysts can surface anomalies where CMS or HHS risk scores are incongruent with the actual risk status of individual members. Palantir allows analysts to visualize these connections and patterns, triage recommendations, and take next steps—whether that is adjusting claims or reaching out to providers. Program Integrity Palantir is a powerful analytical platform for detecting fraud, waste, and abuse across all stages of the program integrity lifecycle, from provider/beneficiary enrollment to criminal prosecution. Palantir integrates all data into a single environment to support lead generation, triage, investigation, and action, allowing analysts to build out complex networks of fraudulent provider groups and identify emerging fraud schemes with unprecedented speed. Using Palantir, analysts can rapidly build out fraud networks.
 Palantir Health Page 6 Page 8
Palantir Health Page 6 Page 8This is a modal window.
